Medicare terms and a brief history
Medicare FAQ
Hello! I’m Niki and I’m the owner and operator of Chicagoland Medicare, a woman-owned, family-run, privately held boutique independent Medicare insurance agency based in the western suburbs of Chicago, Illinois. We serve Medicare beneficiaries in Illinois, Indiana and Wisconsin.
We encourage clients to review their insurance plan every year
If You’re not Reviewing Your Medicare Coverage Every Year, You’re Probably Paying Too Much!
We Help You Customize Your Medicare Insurance
At some point, you and every other American close to or on Medicare will want the same thing—help! Help knowing when and how to sign up for Medicare. Help avoiding lifelong Medicare enrollment penalties. Help understanding Medicare insurance coverage options. Help deciding which Medicare insurance plan is “best.” Help shopping for and buying Medicare insurance policies. Help finding a Medicare insurance agent (that’s us!). Help reviewing Medicare insurance coverage annually.
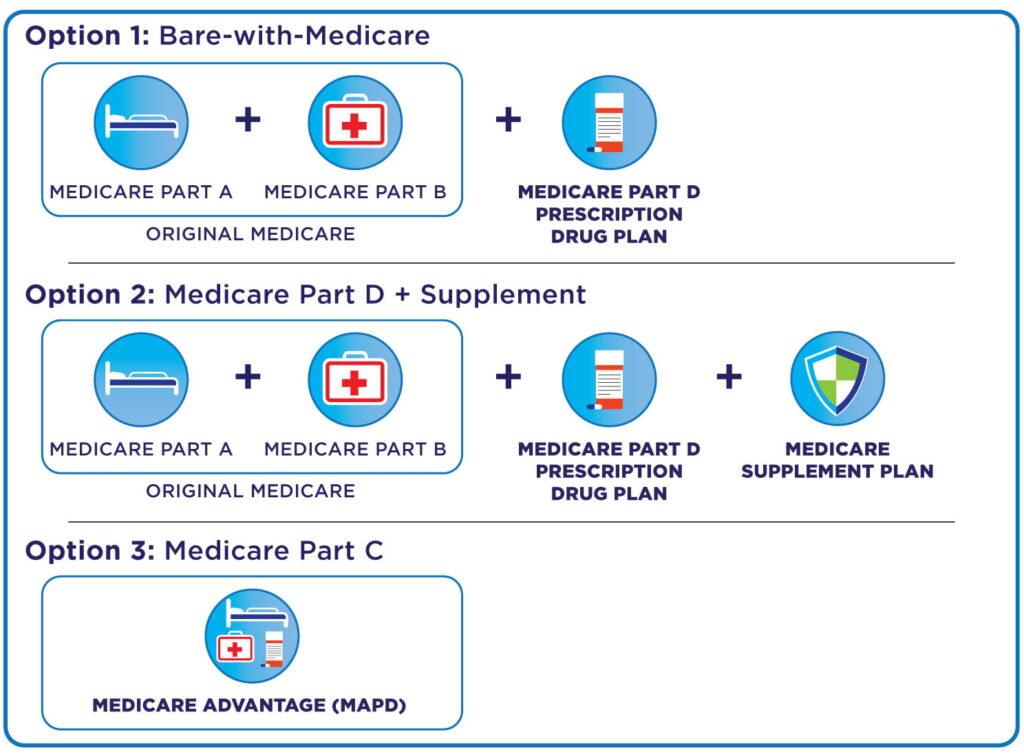
If you buy the “wrong” type of Medicare insurance and then decide it’s not the best path for you, you may not be able to buy the “right” choice later on. Just because you made a choice at age sixty-five, doesn’t mean it’s still the right plan when you turn seventy.
Once you do make a choice, you’re generally locked into that choice for an entire year.
Making the wrong Medicare insurance choice can cost you thousands of dollars, even tens of thousands of dollars.
When you buy Medicare insurance, you have hundreds and perhaps thousands of Medicare insurance coverage choices to choose from. Choosing which of the three paths is right for you can be confusing. Once you choose a path, it gets even more complicated because the number and combination of Medicare insurance policies you can buy in either option can be absolutely dizzying.
That’s where Chicagoland Medicare comes in! Call or click to create an appointment today!
There Are Gaps in Original Medicare Parts A and B. The Right Medicare Insurance Plans Can Solve:
- Private hospital room or private nursing in the hospital
- Healthy food dollar amount allowances at grocery stores
- Adult daycare visits and personal home helpers
- Lifestyle drugs, including erectile dysfunction prescriptions
- Air conditioner allowances for people with COPD and asthma
- Transportation to doctor’s appointments
- Nutritional programs, personal trainers, and access to spas
- Grocery delivery
- Flexible dollar amount allowances for healthcare-related items at select retailers (sometimes in the hundreds of dollars per year)
- Acupuncture and massage therapy
- Gym memberships or fitness classes
- Weight management programs
- Dental insurance and dentures
- Routine eye exams and glasses
- Routine hearing tests and hearing aids
- In-home safety assessments and services
Medicare Terms
Select each Question to reveal additional information:
Medicare part D
The tiers and Phases of Medicare Part D
benefit phases of Medicare Part D Prescription Drug Plan:
Medicare sets a “standard” or “minimum” Medicare Part D Prescription Drug Plan design for insurance companies to offer. Many offer plans that cover the gaps outlined below, usually for a higher premium.
There are four benefit phases of every “standard” Medicare Part D Prescription Drug Plan, and they reset every year on January 1. This isn’t something you can pick or change; it’s what the federal government decided was the way these would work. However, Medicare insurance companies can offer better benefits than just the standard plans, and many do. For example, there are many plans for sale that eliminate the deductible in Phase 1 but still follow this four-phase approach.
A byproduct of this four-phase approach is that, very likely, you won’t pay the same amount for the same prescription at the pharmacy for the entire year. It’ll be a moving target as you wander through these stages, so don’t be surprised. There’s nothing for you to track; the Medicare insurance company tracks all of this for you. You may be able to use mail-order to get lower prices, and of course, check other in-network pharmacies.
PHASE 1—This is the deductible phase. In 2023, you pay 100% of your prescription costs until you are at $505 out-of-pocket. This amount goes up every year, sometimes a little, sometimes a lot. Again, there is good news—there are a number of Medicare insurance companies that offer plans with zero deductible.
PHASE 2—This is called the Initial Coverage period. In 2023, after Phase 1, you pay a copay for each prescription until the total drug costs (what you and the Medicare insurance company spend, including any deductible) reach $4,660. This also typically goes up every year.
PHASE 3—This is called the Coverage Gap or “doughnut hole” and kicks in when the total prescription spending is between $4,660 – $7,400 (2023). This stage has really improved for consumers over the last few years. The insurance company doesn’t pay any benefits at this stage, but you get discounts from drug manufacturers and the government during this stage. You exit the coverage gap when your total out-of-pocket cost on covered drugs (not including premiums) reaches $7,400 for the year. Your out-of-pocket cost is calculated by adding together all of the following: yearly deductible, coinsurance, and copayments from the entire plan year, and what you paid for drugs in the coverage gap (including the discounted amounts you didn’t pay in that stage). There’s nothing for you to do or track here.
PHASE 4—This is called the Catastrophic Coverage phase. Once your out-of-pocket cost totals $10,516.25 (2023) in a given year, you exit the gap and get catastrophic coverage. In the catastrophic stage, you will pay a low coinsurance or copayment amount (which is set by Medicare) for all of your covered prescription drugs. That means the plan and the government pay for the rest—about 95% of the cost. You will remain in this phase until January 1 of the next year.
Medicare Part D Tiers:
Within the formulary, prescription drugs will be categorized into tiers. These tiers are usually labeled 1-5, each with different copays or coinsurance amounts. Tier 1 drugs are usually the cheapest, Tier 5 the most expensive.
Tier 1: Preferred Generics
Tier 2: Non-preferred Generics
Tier 3: Preferred Brand Drugs
Tier 4: Non-preferred Brand Drugs
Tier 5: Specialty Drugs
Formulary tiers vary from plan to plan; sometimes, they come with six tiers. Soon, Medicare is expected to allow seven tiers.
Medicare Part D Prior Authorization
Medicare insurance companies may require your doctors or other health providers to prove you need certain drugs before you can fill a prescription at the pharmacy. To do this, the insurance company could ask them to submit their medical reasoning, medical history, lab results, current symptoms, and treatment history. Most, if not all, Medicare Part D benefits have a Prior Authorization component, but the drug categories and individual drugs within the programs vary by company and the plan they’re on. There are two types of reviews: Standard and Expedited. If you’re having trouble getting approvals or need the review to happen quickly, you may want to specifically ask for an Expedited Review.
Prior Authorizations are typically found on brand-name prescription drugs that have a generic option available, drugs that have the potential to be abused, drugs used for cosmetic reasons, drugs that may have adverse health effects, or that are dangerous when combined with other medications.
Medicare Part D Networks
Most Medicare Part D plans will come with a preferred network and a non-preferred network, although what they call them might be different. Get your prescriptions from preferred pharmacies and your costs will be lower. Get them from non-preferred pharmacies and they’ll be higher. Essentially, insurance companies contract better pricing (for them and often, for you) with those preferred brick-and-mortar or mail-order pharmacies and do not get the same deals with non-preferred pharmacies.
Sound confusing? It kind of is–until you get used to it. There are a few things to remember:
- Each Medicare insurance company selling Medicare Part D Prescription Drug Plans must offer at least the minimum plan design described above. A large number of them also sell enhanced plans that eliminate the deductible and provide additional coverage through stages 2-4.
- Each Medicare insurance company tracks the four phases as you go through them for you. There’s nothing for you to do or track.
- Benefits reboot every January 1 for all Medicare Part D Prescription Drug Plans. (They also reboot January 1 for Prescription Drug Plans embedded into a Medicare Advantage plan, too.)
- There is no 4th quarter “carry-over” feature like some employer-based health insurance plans have. So, if you were used to getting “credit” in the following year for paying deductibles or co-insurance in the 4th quarter in the prior year, Medicare doesn’t do that. Hypothetically, you could pay your deductible on December 31 and then pay it again on January 1.
- Each insurance company has its own formulary, which is a list of drugs they cover on their plan. No two companies have the exact same one, but Medicare makes them cover at least two drugs in each “class” of medications that treat a condition. They might not be the drugs you take, but some companies might cover yours. Yes, they change the drugs covered in the formularies and also change how much they cost every year. That’s why it’s important to make certain you check every October to see if you’re still in the best plan for you.
- Each insurance company has its network of preferred, or “in-network,” pharmacies you can go to. Many have “preferred” and “non-preferred” lists, and you’ll get the best bang for your buck at the “preferred” pharmacies. Why? Essentially, insurance companies contract better pricing (for them and often, for you) with those preferred pharmacies and do not get the same deals with non-preferred pharmacies.
- Many insurance companies offer mail-order prescription delivery, and it’s often cheaper than filling them at your local pharmacy.